Acute gastritis with psychiatry opinion
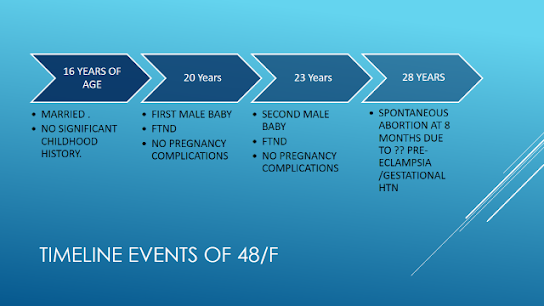
Case of 46 year old female diagnosed with functional bowel disease with history of tobacco use and attention seeking
June 24,2021
This is online E-log book to discuss our patient’s de-identified Health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s Problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence-based inputs. This is the E-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of" patient clinical data analysis” to develop my competency in reading and comprehending clinical data Including history,clinical findings ,investigations and come up with diagnosis and treatment plan.
This is a case of 46 year old female diagnosed with functional bowel disease with history of H/O tobacco use & Attention Seeking
(History taken from pt with help of translator [pt son]
Admitted in summer 2021 (day 1 )
Day 2
CHIEF COMPLAINTS:
- Pain abdomen since 2-3 months
- Abdominal distension since 1 month
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic/normal 12 yrs back then she had history of fall due to slip while she was carrying a load of water to her home following which she developed low back ache radiating to legs subsided after taking medications.
Since 2-3 months she had pain abdomen which is gradual onset, not associated with nausea/vomiting, no h/o weight loss, no loss of appetite, no easy fatiguability.
Since 1 month she observed abdominal distension, which is insidious onset ,gradual and not associated with constipation, no obstipation, no decreased urine output.
N/k/c/o HTN,DM,BA,TB.
TREATMENT HISTORY:
Not significant
PERSONAL HISTORY:
• Married
• Homemaker/farmer
• Normal appetite
• Mixed diet
• Regular Bowel movements
• No known allergies
• Tobacco consumption
FAMILY HISTORY:
Not significant
PHYSICAL EXAMINATION:
Pallor: -
Icterus: -
Cyanosis: -
Clubbing: -
Koilonychyia: -
Lymphadenopathy: -
Edema: -
VITALS:
BP: 140/90 mmHg
PR: 76 bpm
RR: 18cpm
Temperature: Afebrile
GRBS: 136mg/dl
SpO2: 99% on RA
SYSTEMIC EXAMINATION
CVS:
S1, S2 heard
No thrills
No murmurs
Resp S:
Trachea centrally located
No dyspnea
No wheeze
Vesicular breath sounds
No Adventitious breath sounds
ABDOMEN:
Shape: Obese
No tenderness
No palpy mass
No bruits
No free fluid
CNS:
Conscious
Coherent
Cooperative
Normal speech
No signs of meningeal irritation
CEREBRAL SIGNS:
None
PROVISIONAL DIAGNOSIS:
Acute gastritis with psychiatry opinion
PLAN OF TREATMENT:
Day 3
• Tab. PAN 40 mg PO/OD
• Tab. MVT PO/OD
• BP/PR/Temp/SpO2 Monitoring 4th hourly
• GRBS 12th hourly monitoring
Day 4
• Tab. PAN 40 mg PO/OD
• Tab. MVT PO/OD
• BP/PR/Temp/SpO2 Monitoring 4th hourly
• GRBS 12th hourly monitoring
Day 5
• Tab. PAN 40 mg PO/OD
• Tab. MVT PO/OD
• BP/PR/Temp/SpO2 Monitoring 4th hourly
• GRBS 12th hourly monitoring
Day 6
• Tab. PAN 40 mg PO/OD
• Tab. MVT PO/OD
• BP/PR/Temp/SpO2 Monitoring 4th hourly
• GRBS 12th hourly monitoring
Day 7
• Tab. PAN 40 mg PO/OD
• Tab. MVT PO/OD
• BP/PR/Temp/SpO2 Monitoring 4th hourly
• GRBS 12th hourly monitoring
INVESTIGATIONS:
• CBP
• CUE
• Blood Urea
• Serum Creatinine
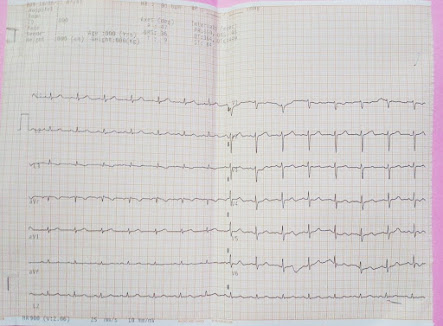
• ECG
• Endoscopy : mild fundal gastritis
• Psychiatry opinion
ECG
Day 2 2:30pm
C/S/B Dept. of Psychiatry
This is a case of 46 year old female diagnosed with functional bowel disease with history of H/O tobacco use & Attention Seeking
(History taken from pt with help of translator [pt son]
C/C -
- Pain abdomen ∵ 2 years
- Abdominal Distention ∵ 3 months
Pt. Says that this did not subside completely after using medication and she did not bother about as could do her daily activities.
3 months back pt. observed pain abdomen of burning type in epigastric region, during which she also observed abdominal distension for which she again consulted doctor. As doctor could not explain them the cause of pain they came to OPD for further treatment.
Pt. Says that her pain subsides on doing work and aggravates during sleep.
Pt. used tobacco since 15 years stopped consuming since 1 month
Pt. Denies any withdrawal symptoms
Pt. denies any H/O
- personal
- occupational
- familial
- sexual
- Financial stressors
- No H/O head injury seizures
- No H/O pervasive low mood suicidal ideas
- No H/O Bizarre belief, self talking, suspiciousness
- No H/O flight of ideas , grandiosity
- No H/O other substance use
- No H/O suspending doom or any other anxiety symptoms.
OD denies any features of
-Self mutilation
-over concern with physical attractiveness
-manipulative behaviour
N/K/C/o HTN, DM, BA , TB
No significant past & family history of psychiatric illness
MSEI - pt looking appropriate to age moderately built dressed appropriately
ETEC +ve sustained
PMA : - ve
Rapport Established (with help of translator)
Speech T -ve. RT -ve
V -ve
R -ve
Relevant & Coherent
Attitude - cooperative
Thought- Preoccupations of health
Perception-NAD
Oriented to T+/P+/P+
HAM-D : 7
HAM-A : 1
Insp: 1) Functional Bowel Syndrome
2) Tobacco Harmful use.
USG Abd :- S
PLAN-
1) Review to PSY OP on Monday for psychotherapy.









Comments